Clinicians: Discover how QTUG™ can help you prevent falls! Older adults: Create your free Kinesis Screen account now!
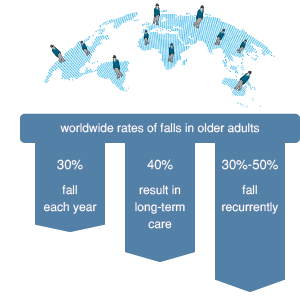
Falls in older adults are a major problem worldwide. An an estimated 30% of adults over 65 years of age fall each year. In the community, the proportion of people who sustain at least one fall over a one year period varies from 28–35% in the over 65 years age group to 32–42% in the 75 years and older age group, with 15% of older people falling at least twice each year (1). Incidence rates in hospitals are higher, and in long-term care settings approximately 30–50% of people fall each year, with 40% falling recurrently (2). The direct and indirect societal costs of falls are enormous. Among older people in the US alone, the cost of falls has been estimated to be in the region of US$30 billion per year (3).
The combination of high frequency and high susceptibility to injury in older people make falls a major geriatric issue in their own right.
Falls in the elderly have been associated with gait and mobility impairment (4), deteriorating postural stability, muscular strength and vestibular function. These deteriorations can manifest as problems in walking and turning (5). Additional risk factors for falls include poor vision, use of psychoactive medications, postural hypotension, environmental hazards and problems with feet and footwear.
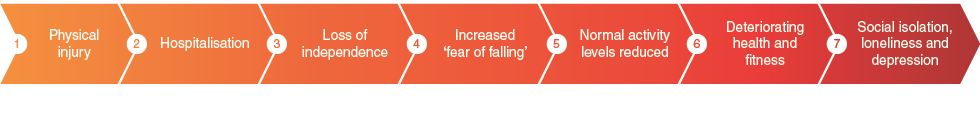
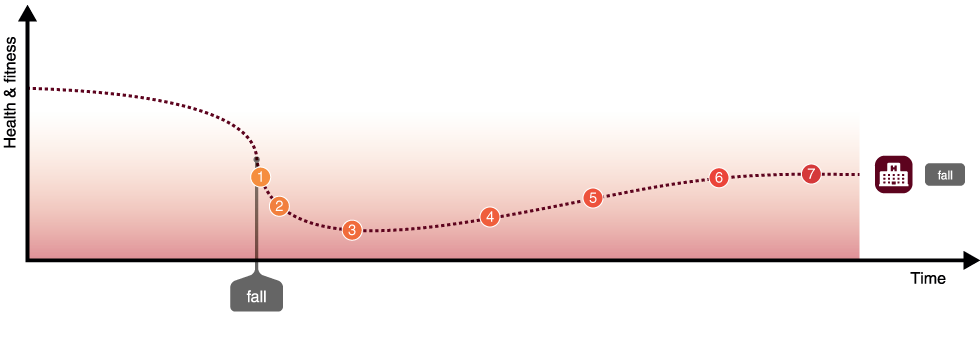
Not only may a fall result in a physical injury to an older person, there is a strong likelihood that the person will lose independence due to hospitalisation and/or a short or long term stay in residential care.
Patients that fall often develop a condition known as “fear of falling”, which can often result in a reduction in the normal levels of physical activity. This results in declining in health and physical fitness which can in turn increase an older person’s risk of falling. In addition to the fear of falling, other psychological issues present themselves, such such as social isolation, loneliness and depression.
Generally, falls prevention activities aim to prevent or reduce the overall number of falls by taking preventative measures; identifying those patients most at risk of falling earlier, and then by providing early and targeted intervention to reduce that risk. It is broadly accepted that falls are not inevitable and can be reduced. All too often however, falls management activities commence after a person has fallen. Falls prevention focuses on people who have previously fallen, in addition falls prevention aims to identify those at risk who have not fallen to stop the first fall and subsequent impact on health and quality of life.
Multifactorial intervention has been shown to be effective in reducing the incidence of falls in community-dwelling older adults although (6-9), despite detailed targeted multifactorial interventions, the best reported reduction in the incidence of falls is in the region of 30%. Accurate identification of those participants at high risk of falls, would facilitate appropriate and timely intervention, and could lead to improved quality of care and reduced associated hospital costs due to reduced admissions and reduced severity of falls.
The ‘Timed Up and Go’ (TUG) test (12-13) is a standard mobility assessment used to screen for balance problems in older people. The TUG test consists of the participant getting up from a chair, walking three metres, turning at a designated spot, returning to the seat and sitting down. The time taken to perform the test is recorded using a stopwatch. Current clinical practice suggests that older adults with longer TUG times are more likely to fall than those with shorter times. The performances of older adults prone to falling can be very different from those who do not fall. Consequently, the TUG test is one of the most widely used tools for identifying patients at risk of falls and has been recommended by the American Geriatrics Society/British Geriatrics Society (AGS/BGS) guidelines (14) as a screening tool for identifying older people at increased risk of falls.
In the U.K., the National Institute for Clinical Excellence (NICE) guidelines (15) on the assessment and prevention of falls state that the TUG test – as referred to in the AGS/BGS guidelines – "is both pragmatic and frequently cited, can be used in any setting, and its administration requires no special equipment". The TUG test is considered to be of clinical value due to the range of functional movements contained within, including the sit to stand transition, the walking phase, the 180° turn portion and the stand to sit transition. The TUG can be administered in any setting. However, the TUG test relies on subjective clinical judgement and the value of timed cut-off values which vary considerable across the literature. Other tests – such as the Berg balance test, Tinetti scale, functional reach and dynamic gait test – may offer more detailed assessment and be of diagnostic value, but take longer to administer and need both equipment and clinical expertise. These tests cannot be recommended for use in all settings and may be more useful during a comprehensive assessment by a multidisciplinary team.
Quantitative methods for estimating falls risk or predicting falls have been suggested as a more objective means to identify patients at risk of falling before a fall, suitable both for use by experts and non-experts. These methods can be used in primary, secondary or residential care settings for assessing and targeting of individuals at high risk of falls.
An objective method for assessing falls risk (using for example wearable sensors), suitable both for use by non-experts and for deployment in a community care setting would find clinical application for screening and targeting of individuals at high risk of falls.
As current methods (e.g. Physical Profile Assessment, Tinetti scale, Berg balance scale) for assessing falls risk and mobility are often driven by a subjective observation of the patient’s gait and mobility there is potential for variability in administration and results.
To address this variability, a new quantitative method for estimating falls risk (identifying patients at risk of falling) has been developed, known as the Quantitative Timed Up and Go (QTUG). QTUG™ (17,18) is based on the Timed Up and Go test and is instrumented with wireless sensors placed on each leg. This technology provides a method for objective assessment of mobility and falls risk. It allows identification of a specific mobility impairment by comparison against a reference population in older adults.
QTUG™ is intended to assist those assessing falls risk, by providing a falls risk score (known as the Falls Risk Estimate (FRE)) along with fast, accurate and objective data. QTUG™ provides an automatic comparison of the patients gait and mobility against average values for their age and gender. QTUG™ also incorporates the American Geriatric Society (AGS) and British Geriatric Society (BGS) falls questionnaire which records standard falls risk-factors (such as polypharmacy, orthostatic hypotension, vision impairment etc). These data are used to improve the statistical falls risk estimate that QTUG™ provides.
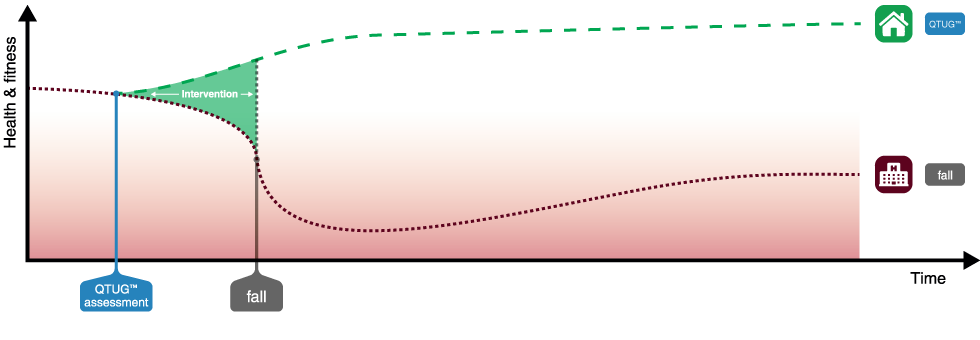
Falls occur as a result of a decline in health and fitness in older adults, which is part of the normal ageing process. By using Kinesis Screen to allow an older adult to self-assess for risk of falls, triggering referral to assessment using QTUG™
to screen for gait and mobility impairment, and identify those at risk, QTUG™ uses the Timed Up and Go (TUG) test and body-worn sensors
to produce a simple falls risk score and identify gait and mobility problems.
This can facilitate early intervention, as a result setting patients on a different path by reducing
a patients' risk of a fall, with the added goal of maintaining independence and allowing the patient to stay in their home and community.
Kinesis Balance™ allows an older adult ot their carer to monitor balance and falls risk at home using a smartphone, allowing them to take action to prevent falls.
Studies have shown that early and targeted intervention can reduce the incidence of falls by 30% - 40% (6-9).
The challenge then becomes identifying those patients at risk of falls.
Recently, NICE, The National Institute of Health and Care Excellence have issued a briefing note on QTUG™ (16).
Click here to read the briefing note.